2023 PFS Conversion Factor
On November 1, 2022 the U.S. Department of Health and Human Services (HHS), through its Centers for Medicare & Medicaid Services (CMS), published its Final Rule for the Calendar Year (CY) 2023 Physician Fee Schedule (PFS). The CY 2023 PFS conversion factor was set at $33.06, a decrease of $1.55 to the CY 2022 PFS conversion factor of $34.61. This conversion factor reflects the statutorily required update of 0% for CY 2023, expiration of the temporary 3% supplemental increase in PFS payments for CY 2022 provided by the Protecting Medicare and American Farmers From Sequester Cuts Act, and the statutorily required budget neutrality adjustment to account for changes in payment rates.
However, at the end of December 2022, Congress passed and the President signed into law the Consolidated Appropriations Act of 2023, which finalized Fiscal Year 2023 appropriations and included several important Medicare policy updates. The bill required changes to the Medicare Physician Fee Schedule conversion factor for 2023. Instead of a 4.5 percent cut to the conversion factor, Congress lowered that cut to 2 percent. With these changes, the conversion factor for this year is $33.8872.
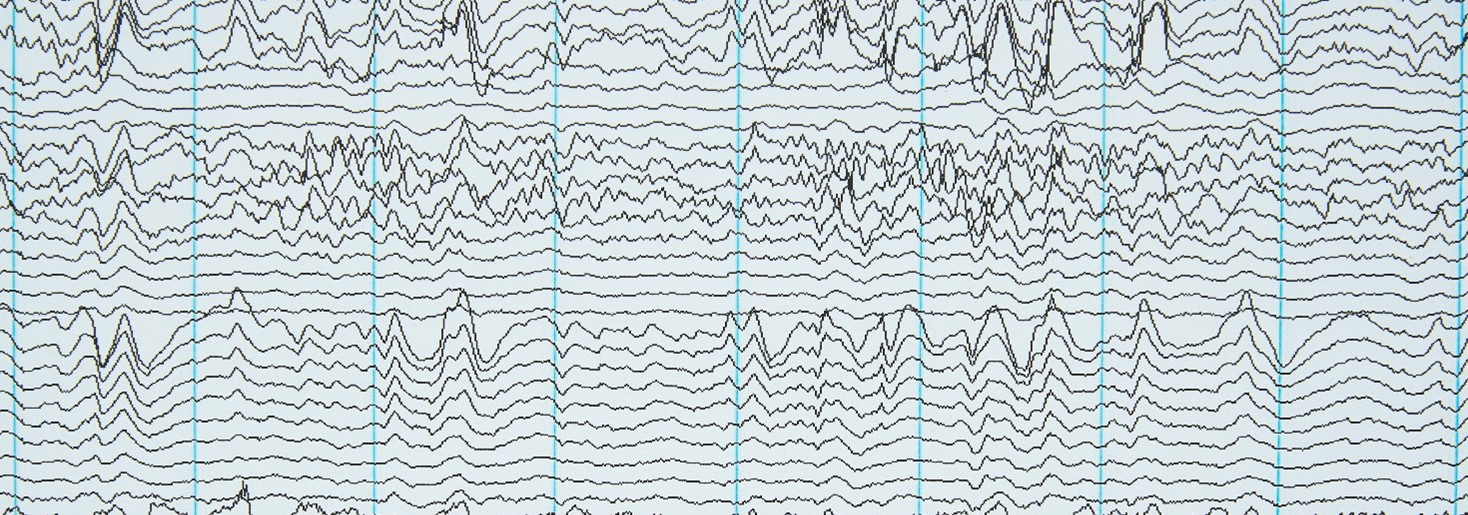
The Long-Term EEG Technical Components
The CPT Codes for Long-Term EEG procedures were completely overhauled for 2020, deleting the procedure codes used for the previous 25 years and replacing them with a new extensive set separating the technical procedures from the professional review and reporting procedures. This was done to address the expanding use of video-EEG studies done in non-facility sites of service (outside of the hospital) and the various levels of monitoring that may or may not be part of the procedures.
CMS has not assigned Relative Value Units (RVUs) to the Technical Codes, due to lack of accurate costing information, particularly related to delivery of the service in the patient home. Therefore, they declared that the reimbursement for the Technical Codes should be set by each of the seven Medicare Administrative Contractors or MACs (there are 12 different MAC areas across the country that process CMS insurance coverage). In 2022, they had yet to establish RVU’s for the Technical Codes. They are classified as status “LC” = Local Carriers price the code. Each Carrier establishes RVUs and payment amounts for these services. To date several MACs have published reimbursement rates for the Technical Codes. These rates vary greatly for example, the reimbursement rate for 95716 (ranges from under $400 per day to $1250 per day). In addition, some national health insurance carriers have also set a wide range of rates.
For more detailed background information on these changes see the blog article: https://corticare.com/corticare-stagin/2020-long-term-eeg-monitoring-cpt-codes-technical-components/
Long-term EEG Technical Component Codes (95700, 95705 – 95716)
The CPT Codes for Long term EEG are defined by the length of time of the long-term recording, whether the study includes the recording of video with the EEG and if there is no monitoring of the study, intermittent monitoring, or continuous monitoring (see Figure 1. Sourced from the NAEC).

The 24-hour period for a study begins at the time it is initiated. This means that a “day” for study may start at 10:00 AM or at 9:30 PM or at 3:00 AM depending on when the recording began. When coding for a multiday study, a partial day code (less than 12 hours) may be applied once to capture the period.
Long-Term EEG Professional Component Codes
The Professional Component Codes are applied based on three factors: EEG study with or without digital video, duration of recording and whether the physician reviews and generates a daily report on a multiday recording or only reviews the study at the end of the recording and generates one final report (see Figure 2. Sourced from the NAEC).

When billing for services, codes 95717 through 95720 require physical access to the data (EEG with or without video) during the recording. They require the generation of a daily report and a final summary report at the end of the study. 95717 and 95718 may be applied once during a multiday recording if a period of fewer than 12 hours is part of the total duration of the recording.
In cases where the physician does not have real-time access during a multiday study (for example an ambulatory EEG study that is not monitored), the study is reviewed and a report is generated after the study is concluded, then Codes 95719 to 95726 are used depending on the length of the study (note 95719 and 95720 may be used for only a 12 to 26-hour recording, studies lasting more than 26 hours but less than 36 hours are billed by adding on the appropriate 2 to 12 hour codes 95717 or 95718).
Non-Facility PFS reimbursement covers procedures performed in a physician office, IDTF, or in the patient’s home by a physician office or IDTF.
2023 CPT Codes and RVUs for Long Term EEG Studies

CPT is a registered trademark of the American Medical Association
Links


